John Wojcik pays tribute to a black US activist who spent six decades at the forefront of struggles for voting rights, economic justice and peace – reshaping US politics and inspiring movements worldwide
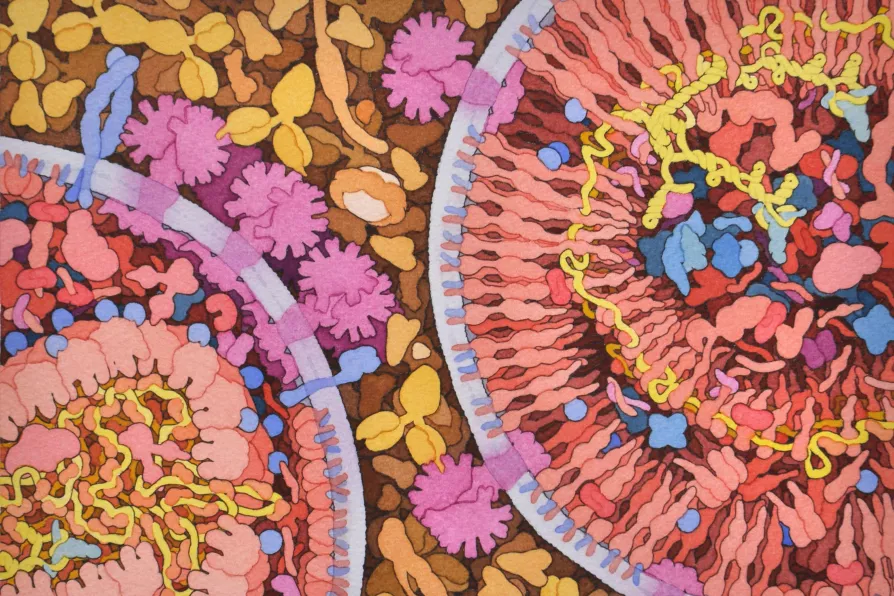
 COMPLEX: Watercolour and ink on paper illustration of HIV maturation. After full assembled virus particles have been released from an infected target cell (usually CD4 T cells, a type of white blood cell found in the immune system), they undergo a process of maturation in order to become fully infectious viral particles.
[David S Goodsell / Welcome Collection / Creative Commons]
COMPLEX: Watercolour and ink on paper illustration of HIV maturation. After full assembled virus particles have been released from an infected target cell (usually CD4 T cells, a type of white blood cell found in the immune system), they undergo a process of maturation in order to become fully infectious viral particles.
[David S Goodsell / Welcome Collection / Creative Commons]
THE development of antiretroviral therapies (ART) has meant that, where available, people living with the human immunodeficiency virus (HIV) now have a normal life expectancy.
Yet despite this achievement, ART is not a cure for HIV and people living with HIV need to keep taking ART for the rest of their life to prevent the development of acquired immune deficiency syndrome (Aids).
As of this moment, two people have been — or at least appear to have been — completely cured of HIV infection, the virus was eradicated from their body and they no longer needed to take ART.

New research into mutations in sperm helps us better understand why they occur, while debunking a few myths in the process, write ROX MIDDLETON, LIAM SHAW and MIRIAM GAUNTLETT

A maverick’s self-inflicted snake bites could unlock breakthrough treatments – but they also reveal deeper tensions between noble scientific curiosity and cold corporate callousness, write ROX MIDDLETON, LIAM SHAW and MIRIAM GAUNTLETT










