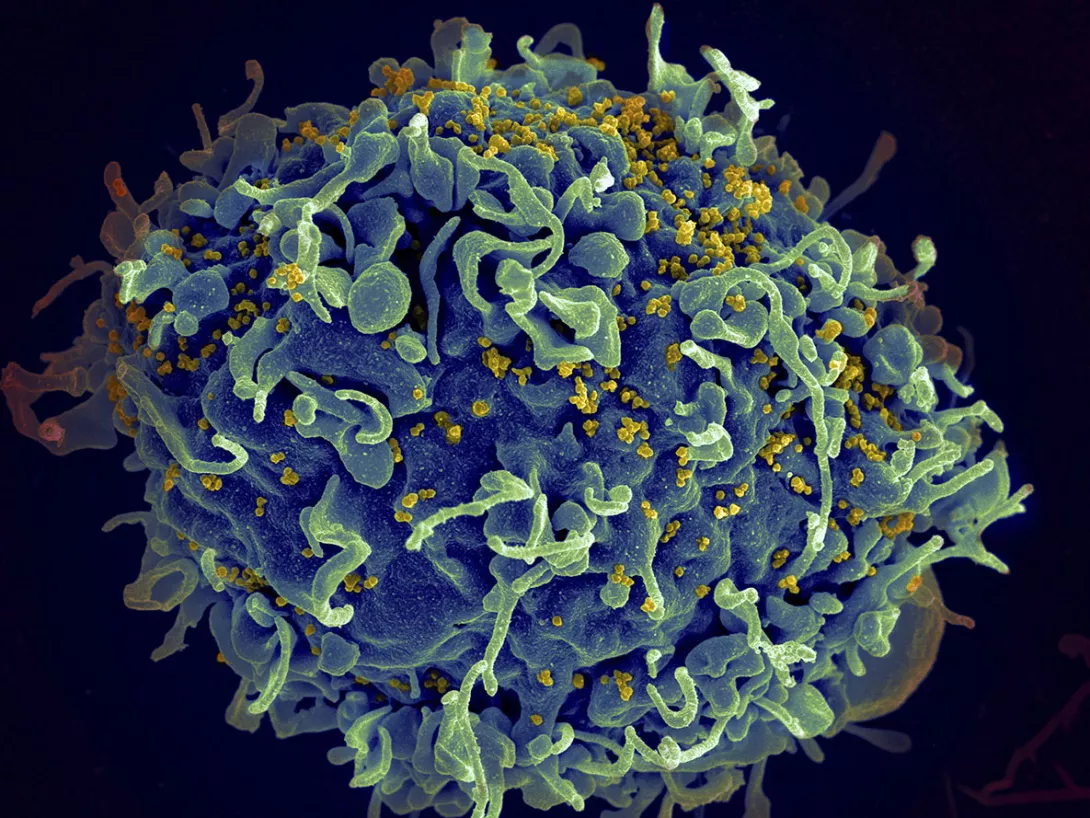
Experts hail 100% effective twice-yearly shot to treat Aids
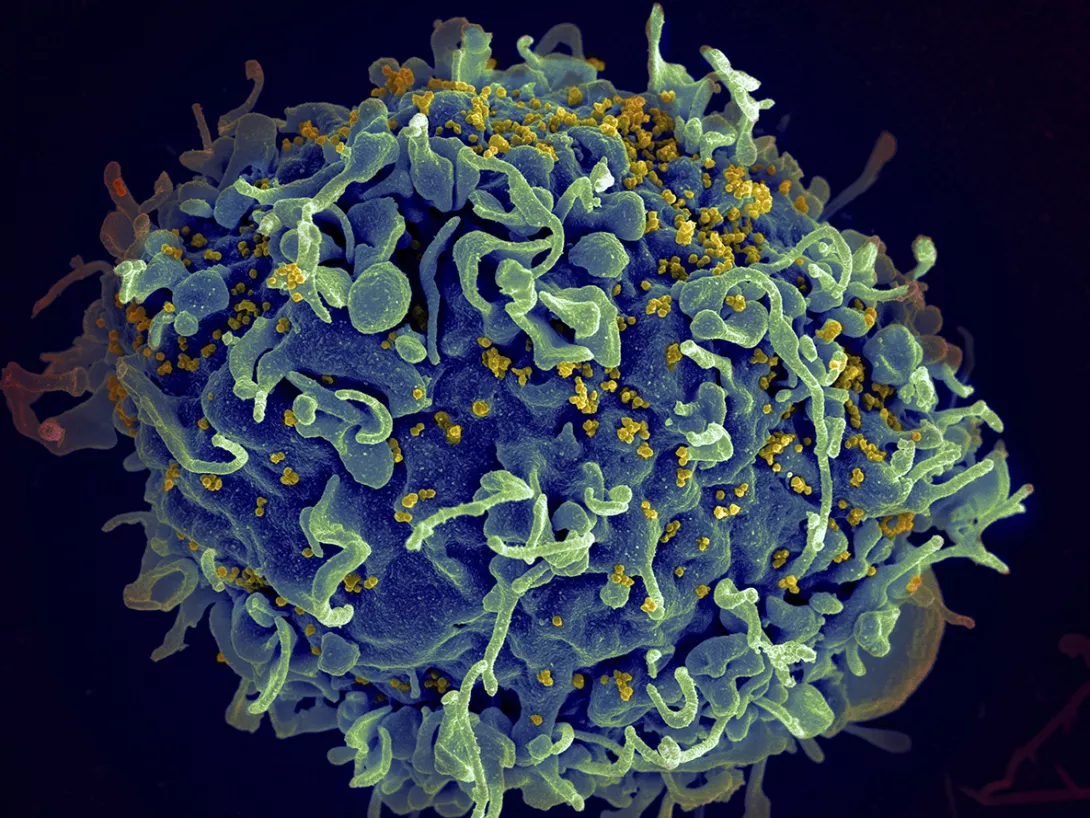
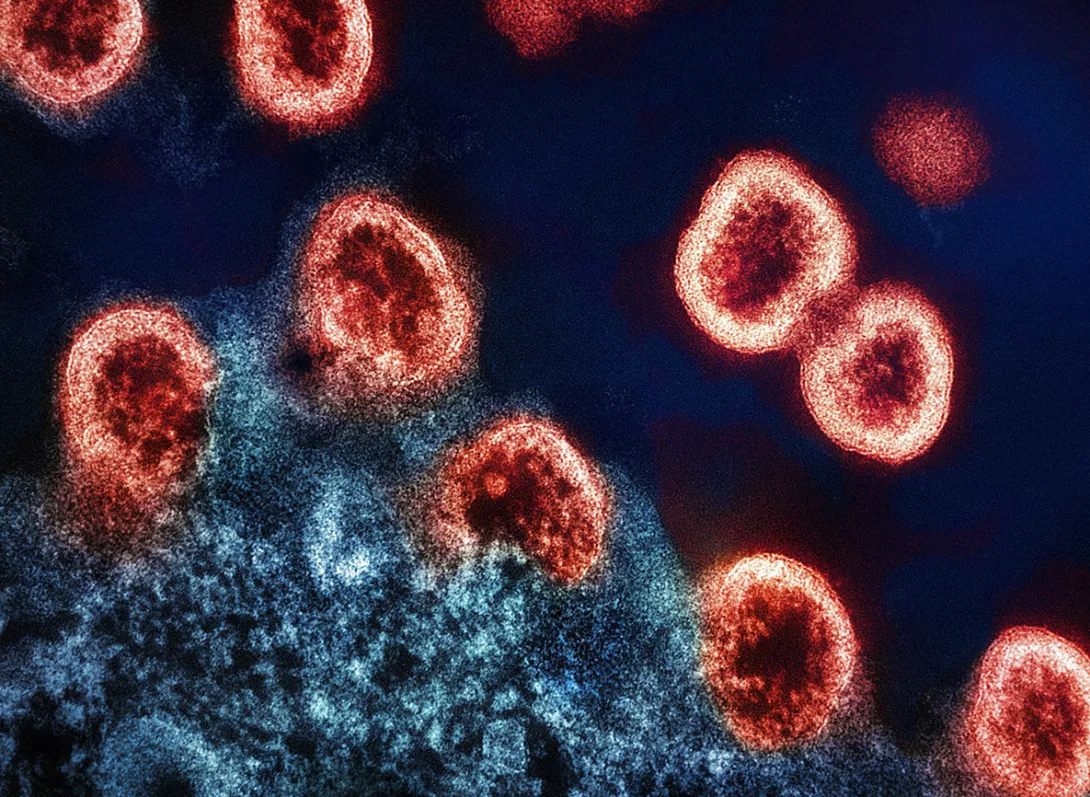
EXPERTS hailed twice-yearly shots used to treat Aids that were 100 per cent effective in preventing new infections in women, according to study results published today.
There were no infections in the young women and girls that got the shots in a study of about 5,000 in South Africa and Uganda, researchers reported.
In a group given daily prevention pills, roughly 2 per cent ended up catching HIV from infected sex partners.
More from this author

ROGER McKENZIE looks back 60 years to the assassination of Malcolm X, whose message that black people have worth resonated so strongly with him growing up in Walsall in the 1980s
ROGER McKENZIE welcomes an important contribution to the history of Africa, telling the story in its own right rather than in relation to Europeans
Similar stories

Despite miraculous trial results showing new treatment could halt transmission, corporate greed and patent laws condemn millions to preventable infection and death, write ROX MIDDLETON, LIAM SHAW and MIRIAM GAUNTLETT
ALAN ROSSI SILVA argues that Gilead’s HIV prevention drug, while promising, highlights systemic failures in the pharmaceutical industry, showing the need to shift towards state-owned drug development and production