Woman whose cancer was missed twice calls for Anne's Rule
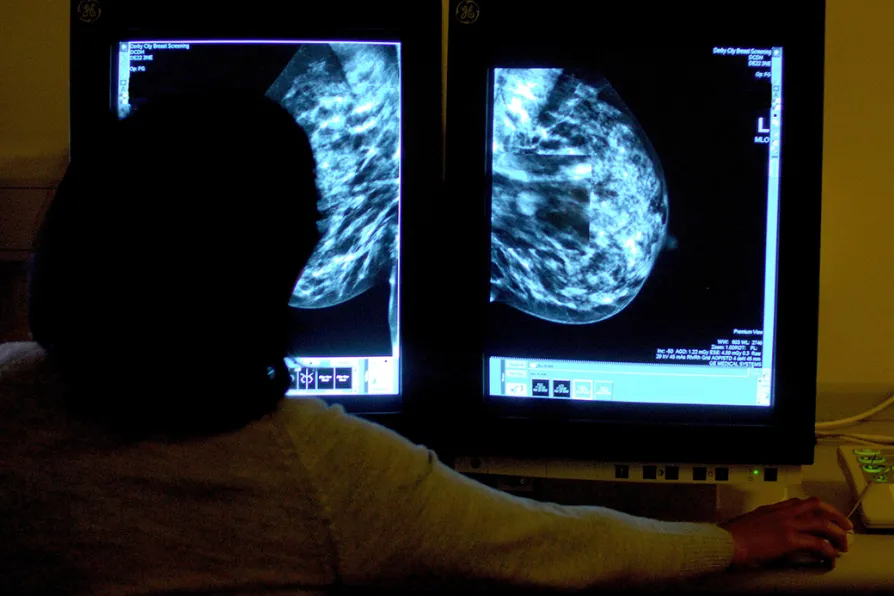
 A consultant studying a mammogram showing a woman's breast in order to check for breast cancer at Derby City Hospital, June 2006
A consultant studying a mammogram showing a woman's breast in order to check for breast cancer at Derby City Hospital, June 2006
A TERMINALLY ill woman whose cancer was missed twice by clinicians is campaigning for the introduction of a change in scan assessments.
Anne’s Rule, as it has been dubbed, would require two radiologists, one of whom specialises in cancer, to check all scan results when clinicians suspect that the disease is present.
At the moment, it is only mammograms — X-rays of the breast used to diagnose breast cancer — that are reviewed by two radiologists as standard practice.
Similar stories














